How dietary changes, Chinese herbs, and other alternative therapies can help treat dogs with AIHA.
Autoimmune hemolytic anemia (AIHA) has been causing significant morbidity and mortality in both humans and animals for at least five decades.1-3 More accurately termed immune-mediated hemolytic anemia (IMHA), this disease is relatively common in dogs.1,2 Excessive or rapid red blood cell (RBC) destruction occurs and is usually due to extravascular causes outside the bloodstream. Intravascular hemolysis from RBC destruction within the blood vessels is less common, but can also occur.3 While conventional treatments can successfully treat and manage AIHA in dogs, an integrative approach that includes both Western and Chinese medicine therapies can be helpful.
DIAGNOSIS CAN BE COMPLICATED
The clinical hallmarks of AIHA are pale mucous membranes from anemia, jaundice, abdominal distention from an enlarged liver and spleen, rapid breathing, cold lower extremities, and sudden collapse.2-5 Confirming the diagnosis can be complicated and controversial.3,4 Testing should reveal the following:
- Auto-agglutination of RBCs in the syringe during blood collection, or in the test tube and a microscopic slide of the blood smear
- Presence of rounded RBCs (spherocytes)
- Usually, a positive direct Coombs test (direct antiglobulin test, DAT).3 Positive DAT signals immune-mediated destruction of RBCs by immunoglobulin G (IgG) and immunoglobulin M (IgM), which binds to the RBC surface.3
Interestingly, a deficiency of regulatory T-lymphocytes does not explain the development of AIHA.5
PREDISPOSING CAUSES
The predisposing factors contributing to AIHA/IMHA in dogs are summarized below:
- Increasing frequency in last two decades
- Sex predilection: twice as common in females
- Breed type predisposition
- Genetic influences associated with 3-5 Major Histocompatibility Complex (MHC Class II) genes
- Hormonal changes: sex, thyroid, adrenal, pancreatic and parathyroid hormones
- Exposures to vaccines; certain drugs (sulfonamides, anti-convulsants); heartworm, flea and tick preventives; allium species (onions, too much garlic); certain houseplants and trees; carpet cleaners, flame retardants
- Underlying diseases: hemangiosarcoma, other cancers, malignant histiosarcoma, leukemia
- Dietary allergies (rare hypersensitivities) and intolerances (more common sensitivities).
CONVENTIONAL TREATMENT
Conventional therapy for AIHA/IMHA depends on a cocktail of immune suppressant drugs and medical management to resolve or control any documented or suspected  triggering causes/events.1,4,6,7 Many veterinarians, including this author, have successfully managed and treated pet patients with severe AIHA/IMHA by using drugs such as corticosteroids, azathioprine, cyclosporine, thyroxine, and novel therapies like extracorporeal plasma exchange.1,4 Blood transfusions with fresh, true universal donor canine packed RBCs (blood type DEA-4), white blood cells, and platelets, as needed, are given when the patients hematocrit (packed cell volume, PCT) falls below 14% to 15%.1,4 Transfusion should not be given until this low level is reached, as it will turn off the bodys own stimulus to make more blood cells.
triggering causes/events.1,4,6,7 Many veterinarians, including this author, have successfully managed and treated pet patients with severe AIHA/IMHA by using drugs such as corticosteroids, azathioprine, cyclosporine, thyroxine, and novel therapies like extracorporeal plasma exchange.1,4 Blood transfusions with fresh, true universal donor canine packed RBCs (blood type DEA-4), white blood cells, and platelets, as needed, are given when the patients hematocrit (packed cell volume, PCT) falls below 14% to 15%.1,4 Transfusion should not be given until this low level is reached, as it will turn off the bodys own stimulus to make more blood cells.
Each case is unique, however, and may be refractory to initial or long term conventional therapy. Serious side effects from these drugs can arise, along with complications such as peripheral and systemic thrombosis (blood clots), pulmonary embolism, and organ failure, especially of the bone marrow, liver, spleen, adrenals, and kidneys. Patients that have been splenectomized are at particularly high risk.1,3,4
ALTERNATIVE THERAPIES FOR AIHA
Alternative remedies and therapies as well as dietary changes have been used successfully in an increasing number of human and companion animal patients. 5-9 If conventional therapies dont work, these alternative approaches can be employed, including those used and taught by holistic veterinarian and naturopathic physician, Dr. Steve Marsden.6,7
Dr. Marsden describes a step-wise approach to therapy that includes:
1. A different perspective: Alternative paradigms to the conventional therapies described above actually predate immune research, and have been shown to successfully treat immune-mediated conditions. The mechanisms involved apparently help control chronic inflammation and immune sensitization.
Chronic tissue inflammation results from the cumulative effects of dietary overconsumption and obesity (where the pet is at least 30% overweight), a syndrome referred to by Dr. Marsden as inflammation dysregulation.
2. Herbal treatment: A successful acute-acting, anti-inflammatory formula for the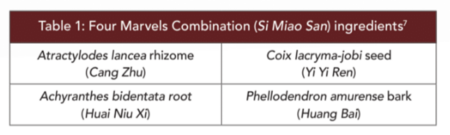 treatment of inflammation dysregulation includes Four Marvels Combination (Si Miao San), very commonly used in veterinary Chinese herbal medicine. (Table 1)
treatment of inflammation dysregulation includes Four Marvels Combination (Si Miao San), very commonly used in veterinary Chinese herbal medicine. (Table 1)
3. Dietary treatment: Dietary therapy is the cornerstone for treating inflammation dysregulation or Damp Heat when viewed from both Eastern and Western perspectives. Chinese medicine tenets state that real food diets are more slowly transported, thereby giving the spleen more time to completely transform them into pure fundamental substances, which means Dampness does not form.
Similarly, an unprocessed diet has been shown to be more advantageous to the body based on biomedical research findings. Processed diets are known to contribute to cardiometabolic disease by mechanisms such as a faster rate of absorption, causing a more rapid rise in insulin levels and more rapid inhibition of AMP-activated protein kinase, leading ultimately to insulin resistance, obesity, and inflammation.6,7
Freeze-drying foods appears to create a tolerable level of processing, and avoids mechanisms that connect metabolism and inflammation. Home-cooked or commercially available real food and raw diets seem to be more anti-inflammatory than freeze-dried diets. However, Chinese medicine views raw diets as too cold for an overly stressed immune system, which may explain why some elderly animals refuse to eat them. While raw diets are well tolerated by most carnivores, some individual animals do not tolerate them. Perhaps the composition of their microbiomes plays a part.
4. The microbiomes role: For several thousand years, Chinese medicine has acknowledged that pathogens invade the body from outside to cause disease unless the body is successfully defended by its Upright Qi, the umbrella of all Qi types that help protect the body against pathogens. It includes our defensive Qi, nutritive Qi, and kidney essence. 7 Kidney essence is the essential foundation underlying the entirety of life, including growth, development, reproduction, aging, and all other functions.
The composition and function of the gut microbiome in people and animals is influenced and controlled by optimizing the expression of genes that benefit and sustain health, while suppressing genes that lead to disease.8,9 As stated earlier, it is also regulated by epigenomic factors, including dietary ingredients, beyond the genes themselves.8
A healthy microbiome protects people and animals throughout life, as it defends against germs, breaks down food to release energy, and produces vitamins. It is present before birth, impacts maternal-offspring health outcomes, maintains the gut-brain axis, and interacts with the immune system.9
5.Brain-gut-skin axis: All types of stress aggravate dysbiosis, the process whereby the normal biosis of the body is disrupted. Dysbiosis impairs bowel wall integrity, which can then lead to T-cell-mediated hypersensitivity.7 Restoring this function, or re-biosis, is necessary to optimize gut and skin functions, brain health and memory.9
In Chinese medicine, dysbiosis is treated with Minor Bupleurum combination (Table 2).  Bupleurum has been shown to reduce depression and anxiety in animal models of repetitive stress. Ginseng is an adaptogenic herb that can normalize and optimize adrenal gland output of cortisol to match the bodys needs. And Scutellaria spp have a long history of use in treating anxiety and other CNS and mood disorders.7
Bupleurum has been shown to reduce depression and anxiety in animal models of repetitive stress. Ginseng is an adaptogenic herb that can normalize and optimize adrenal gland output of cortisol to match the bodys needs. And Scutellaria spp have a long history of use in treating anxiety and other CNS and mood disorders.7
6. Microcirculation: Microcirculation is a blood deficiency and stasis model. Aberrant microcirculation patterns were elucidated in modern medicine just 30 years ago, and are now recognized as playing a central role in disease pathogenesis. Chinese medicine understood this function long ago, with its reliance on pulse diagnosis to guide acupuncture treatments, massage, and the prescription of body movement in the treatment of disease. Over 1,700 review articles cited in the PubMed database describe how disturbed microcirculation lies at the core of degenerative, neoplastic, and inflammatory pathologies.
In Chinese medicine, the liver controls microcirculation and acts as a storehouse of blood to serve and distribute peripheral circulatory needs. A recent excellent review of liver functions, including its detoxifying properties, was published by holistic veterinarian Dr. Ihor Basko.10
The liver functions by coursing and draining the Qi, which is the motive force of the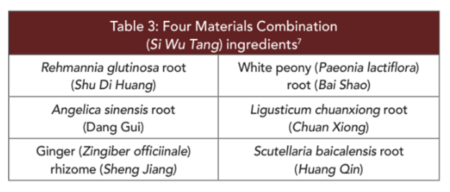 blood. Table 3 lists a widely used Chinese herbal formula for tonifying and moving the blood.
blood. Table 3 lists a widely used Chinese herbal formula for tonifying and moving the blood.
When Qi is not flowing, a thin, wiry vasoconstricted pulse is noted. If the vasoconstriction persists and congestion becomes physically visible or consequential, the patient is experiencing blood stasis.
When treating dogs with AIHA/IMHA, its worth considering the alternative modalities outlined in this article, especially if the patient isnt responding well to conventional therapy, or is experiencing side effects or complications.