Why CST is a valuable tool for the equine cancer patient.
Cranial sacral therapy (CST) has shown efficacy in treating inflammatory bowel disease, migraines, post-traumatic stress disorder, cranial skeletal trauma, concussion, and psychological disorders such as depression in humans. It is also an effective tool to use in conjunction with other modalities during cancer treatment.
In veterinary applications, CST offers a way to decrease the side effects associated with chemotherapy or radiation. And following surgical interventions, especially in the equine where induction, movement and recovery are not without physical and structural risks, CST and osteopathic manual manipulation can be especially beneficial.
History of osteopathy and cranial sacral therapy
Osteopathy began in the 1850s when Dr. Andrew Taylor Still observed how the motion of the body’s structures correlated with overall health. He proposed that by manipulating the structures of the body to create optimal motion, the overall autonomic function of the body could be improved, and the body could be supported to correct itself and heal.
 Dr. Still introduced the concept of “terrain”, an area of the body adversely affected by immobility in bones that border the blood supply, lymphatics and nervous structures to a particular area. This can result in congested capillary beds, increased contraction in muscles, decreased viscosity in the serum surrounding the fascia, and/or hypersensitization of the nerves — all of which have an effect on overall tissue vitality in an area and can lead to degeneration, injury and illness.
Dr. Still introduced the concept of “terrain”, an area of the body adversely affected by immobility in bones that border the blood supply, lymphatics and nervous structures to a particular area. This can result in congested capillary beds, increased contraction in muscles, decreased viscosity in the serum surrounding the fascia, and/or hypersensitization of the nerves — all of which have an effect on overall tissue vitality in an area and can lead to degeneration, injury and illness.
Osteopathy is divided into three major areas: structural manipulation, visceral manipulation, and cranial sacral manipulation. An osteopathic manual manipulation treatment (OMM) that includes all three of these pillars of therapy is considered the most effective.
In cancer patients, structural and visceral manipulation may be limited because of risks associated with metastasis. Many cancer patients (animal and human) suffer side effects associated with cancer therapies while also requiring the best functioning immune system possible. CST can be a great tool to both reduce the side effects of conventional therapies and support the overall health of the immune system. Studies have shown that even a single osteopathic session can dampen the acute stress response in healthy individuals by affecting the autonomic and neuroendocrine response, lowering cortisol and decreasing the sympathetic response. CST can result in less muscle contraction and cramping, reduced drying out of fascia, and less congestion in the periphery, allowing the body’s responses to be directed more towards digestion and healing.
A retrospective look at the use of OMM for inflammatory bowel disease in 2014 showed positive outcomes in treating irritable bowel syndrome, another common sequelae to many cancer treatments. Other research has shown a direct effect on cerebral tissue oxygenation and on migraine headaches thanks to cranial sacral osteopathic techniques. Applying this research to animals demonstrates how we can provide optimal palliative care, minimizing side effects and pain and boosting overall immunity, with the help of osteopathic therapies, including cranial sacral techniques.
 Cranial sacral therapy was first discussed by Dr. William Sutherland in the early 1900s. He published the first explanation of his theories during the 1940s in The Cranial Bowl, in which he explained the anatomy of the human skull. He felt a palpable “filling” and “emptying” motion of the skull that seemed to occur regularly, eight to 12 times per minute, in human beings. He was able to use light manual therapeutic techniques to influence and decrease asymmetries in this movement. Since then, John Upledger, John Martin Littlejohn, and recently, Tad Wanveer in his book Brain Stars, have added to our understanding of cranial sacral therapy.
Cranial sacral therapy was first discussed by Dr. William Sutherland in the early 1900s. He published the first explanation of his theories during the 1940s in The Cranial Bowl, in which he explained the anatomy of the human skull. He felt a palpable “filling” and “emptying” motion of the skull that seemed to occur regularly, eight to 12 times per minute, in human beings. He was able to use light manual therapeutic techniques to influence and decrease asymmetries in this movement. Since then, John Upledger, John Martin Littlejohn, and recently, Tad Wanveer in his book Brain Stars, have added to our understanding of cranial sacral therapy.
The motion that can be felt in the skull has been called the Primary Respiratory Mechanism (PRM) or the Cranial Rhythmic Impulse (CRI). Using Doppler, a measurement was made to compare CRI to the Traube-Hering-Mayer oscillation, the cyclical change in arterial blood pressure, and it appears to be measurable and similar. Further study using Doppler flow was able to show a statistically significant lowering of frequency following cranial sacral manipulation. The authors of the research proposed that cranial sacral therapy affected the autonomic nervous system and lowered blood flow, since the low frequency oscillations associated with the Traube Hering Mayer oscillation appear to be associated with the autonomic nervous system as well. A recent study in veterans showed that osteopathic therapy consisting of visceral, neural and cranial manipulation improved visual and motor accuracy, increased range of motion, decreased pain and improved sleep patterns.
Treating the horse with cranial sacral osteopathy
As an equine veterinarian, I am keen to apply the same principles to my patients. I see many horses presenting with traumatic injuries affecting the head, jaw or first few cervical vertebrae. I am sure the same can be seen in small animal practice. Cranial sacral therapy in these cases may help decrease pain, improve overall range of motion, and possibly change the behavior of the animal when responding to requests from his owner or trainer. In addition, CST may decrease terrain and improve vitality of the overall body.
In equine practice, our exposure to cancer is somewhat minimal, primarily involving skin tumors, benign hypoplasia of the pituitary gland, and occasionally lymphoma. Treating these would include minimal structural work near the tumor, along with CST.
A review of anatomy: paired, unpaired and sutures
The equine skull is made up of paired (parietal, temporal, frontal) and unpaired (occipital, sphenoid, ethmoid) bones; paired bones should move together in synchrony. The portion of the skull surrounding the brain is the the most important, but all the bones will be mobile, and a restriction in a suture between any two bones can cause asymmetry. The smallest restriction is often the one causing the largest problem. The most important of these for motion is the joint between the occipital bone and sphenoid bone on the base of the skull, the spheno-basilar synchondrosis, or SSB. There are many other bones in the skull that can indirectly affect the mobility of the brain case: the unpaired vomer bone at the level of the nasal septum, and the paired maxillary, incisive, pterygoid, palatine, lacrimal, zygomatic, and nasal bones and mandibles. The hyoid cartilages also play a role in the mobility of the skull and cervical spine.
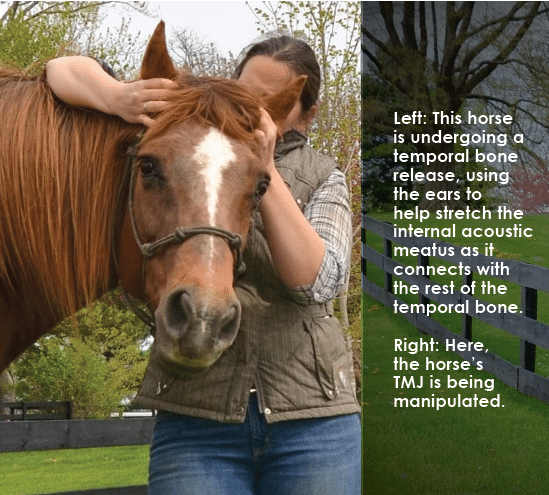
The most common areas affected in horses are the temporal bones, occipital bones, parietal bones and mandibles. When a restriction is found in a suture between two bones, it is usually corrected using a distraction or spread technique to open up the area and decrease tension at the level of the suture line. Depending on the angle of the suture, this can be directly or indirectly applied, possibly in one to two different directions.
An example of an easy one-direction suture that can be manipulated would be the lacrimal suture between the lacrimal bone and maxillary bone. If a horse has mild ocular discharge that necessitates flushing of the lacrimal duct, a distraction of the lacrimal suture could help to open up the duct within the sinus cavity, yielding improved drainage from the eye into the lacrimal duct, and through the duct to the nasal opening at the level of the nostril.
A more complicated suture to release is the squamous suture, lying between the parietal and temporal bone. This suture has a slanted joint. In order to mobilize it, the parietal bone must be manipulated medially and then dorsally to release it, using a squeezing and lifting motion instead of a simple spreading of the suture.
Animal-specific considerations
When it comes to animals, we must deal with patients that will probably not lie down and meditate during the procedure, so creative hand placement may be necessary as he moves his neck and head. However, in this author’s experience, most animal patients will relax and quiet themselves during therapy.
The most sensitive areas appear to be related to the temporal bones and the ears. This is most likely due to multiple cranial nerves with sensory innervation to different portions of the ear. If the animal has a restriction to the cranial base (skull, TMJ, first three cervical vertebrae), it can manifest as a reactive or sensitive ear. Sometimes, mobilization of the occipito-mastoid suture or parietal suture can decrease the ear sensitivity. Often, an immobility in the TMJ will also have a component related to the SSB. Mobilizing the jaw can be helpful, but for full mobility in the TMJ and poll, the SSB will need to be addressed as well.
In conclusion, cranial sacral therapy can be a relaxing and easy way to start your therapy on any animal, and can be helpful in cases where structural or visceral work could be dangerous (in the case of metastasis) or too intense (in the older, debilitated patient). It can also be a great way to help with very young animals, in whom light touch is likely to be safer. It can be effective in cases of trauma to the head, including concussive force injuries. More research needs to be done in humans to assess efficacy for other symptoms and diseases, and since very little research in clinical veterinary medicine has been published, similar studies need to be conducted in veterinary circles.
References
Biondi. “Cervicogenic headache”, JAOA, Vol 100, No 9. September, 2000. S7-S14.
Pujol, Lynnete A. Menefee and Daniel Monti. “Managing Cancer Pain with Non-pharmacologic and Complementary Therapies”. JAOA, Vol 107, No 12. December 2007 ES15-ES21.
Wanveer, Tad, “Brain Stars: Glia illuminating craniosacral therapy”. Upledger Productions, 2015.
Sergueef N, Nelson, KE, Glonek T. “The effect of cranial manipulation on the Traube-Hering-Mayer oscillation as measured by laser-Doppler flowmetry.” Altern Ther Health Med, 2002 Nov-Dec;8 (6); 74-76.
Nelson KE, Sergueef N. Lipinski CM. Chapman AR, T. Glonek. “Cranial rhythmic impulse related to the Traube-Hering-Mayer oscillation: comparing laser-Doppler flowmetry and palpation.” JAOA, 2001 mar;101 (3); 163 -173.
Shi X. Rehrer S, Prajapati P, Stoll ST, Gamber RG, HF Downey. “Effect of cranial osteopathic manipulative medicine on cerebral tissue oxygenation.” JAOA, 2011;111 (12); 660-666.
Christine DC. “Temporal bone misalignment and motion asymmetry as a cause of vertigo: the craniosacral model.” Altern Ther Health Med, 2009 Nov-Dec;15 (6); 38-42.
Downey Pa, Barbano T, Kapur-Wadhwa R, Sciote JJ, Siegel MI, MP Mooney. “Craniosacral therapy: the effects of cranial manipulation on intracranial pressure and cranial bone movement.” J Orthop Sports Phys Ther. 2006 Nov;36(11); 845-853.
Wetzler, Gail, M Roland, S Fryer-Dietz, D Dettman-Ahern. “CranioSacral Therapy and Visceral Manipulation: A New Treatment and Intervention for Concussion Recovery.” Med Acupunct, 2017 Aug 1; 29(4): 239-248.
Vluggen, Janek, DO, MRO-EU, EDO. Cranial Sacral Osteopathy. November 2010.
Budras, Klaus-Dieter, WO Sack, Sabine Rock. Anatomy of the Horse, Schlutersche Verlagsgesellschaft mbH and Co. 2009.








