Treating compulsive disorders in cats can be challenging, and requires an integrated, multidisciplinary approach to achieve the best outcome.
Like humans, cats may demonstrate behaviors typical of obsessive-compulsive disorders (OCDs). Since cats are complex creatures with unique nuances and behaviors, how do we know whats normal and when to be concerned? What does an integrative approach to treating feline compulsive behaviors involve, and why is it the best option when dealing with these complex behaviors?
WHAT ARE FELINE COMPULSIVE DISORDERS?
Feline compulsive disorders are rare, but they can be very disruptive and harm the human animal bond, significantly decreasing quality of life of both cat and owner.
Compulsive disorders involve constant, time-consuming, repetitive, exaggerated behaviors without apparent purpose. It can be difficult to diagnose compulsive disorders because the symptoms originate from normal behaviors. The compulsive nature of the behaviors, their frequency and longevity, their occurrence out of context, and the difficulty involved in interrupting them, are what cause concern. It is important to note that not all repetitive behaviors are compulsive.
HOW DO COMPULSIVE DISORDERS PRESENT IN CATS?
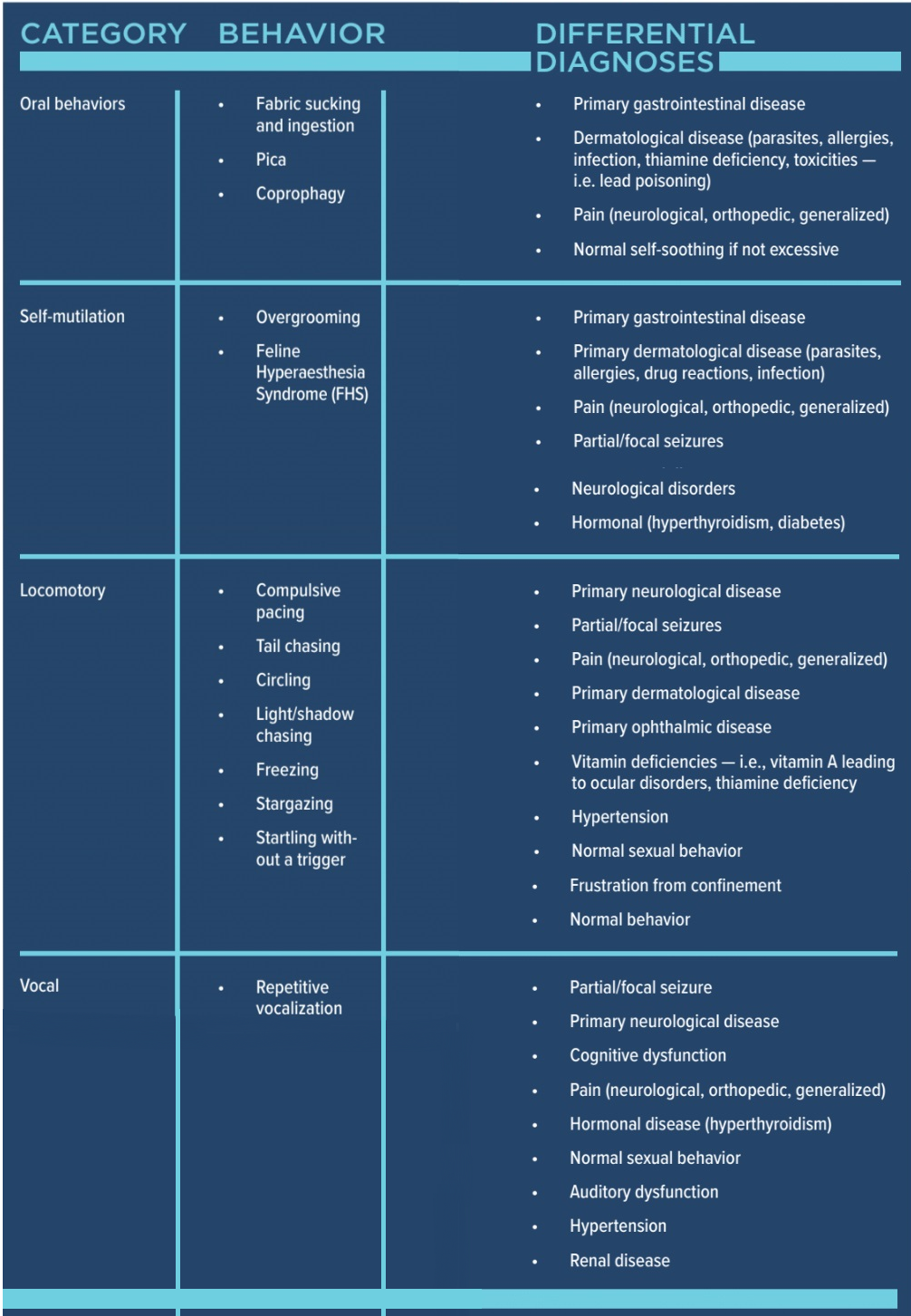
The most common compulsive disorders in cats are oral behaviors, self-mutilation, locomotory disorders and vocal disorders. To the right is a table of behaviors and their differential diagnoses for consideration.
DIAGNOSIS OF COMPULSIVE DISORDERS IN CATS
Diagnosis is based on the cats signalment, a detailed medical history, and exclusion of other diseases.
Signalment breed, age, and neutering status
Oriental breeds are more likely to suffer from true compulsive disorders, with a typical onset of two to eight months of age. Consider the case of a female kitten, four to six months of age and yet to be spayed, with sudden vocalization. She is likely to have reached sexual maturity and be displaying normal sexual behavior. To a first-time cat owner, however, this can appear quite distressing and be misconstrued as significant illness.
Older cats with a sudden onset of excessive, repetitive vocalization should be investigated for hypertension, visual deficits, auditory dysfunction, hyperthyroidism, and cognitive dysfunction. Considering the time of day or circumstances in which the behavior initiates is also often useful; e.g. an older cat yowling and pacing at night is likely to be anxious, in pain, or having visual disturbances (such as night blindness). Differentials including hyperthyroidism and/or hypertension should be considered.
History
It is vital to get a good history to gain a diagnosis and identify any triggers for compulsive behaviors. A thorough history can also guide any necessary further testing, and solidify your diagnosis before constructing your treatment plan. Questions to ask in the consult room include:
- Does your cat go outside?
- Do they come into contact with other animals, wild or pets?
- Has the cat been to a cattery?
- Do you see your cat grooming frequently, often until the hair is thinning and the skin red or bleeding?
- Do you notice your cat scratching a lot?
- Are they up to date with antiparasitic medication? What types of antiparasitics are used, how are they administered, and how often?
- Does your cat have a history of skin disease, excessive itching, or dietary problems?
- Have you changed their diet?
- Is your cat on any medications or being treated for any other illnesses?
- Do they move around your home as normal, jumping onto surfaces like windows as they always have, or has this changed?
- Are there any other symptoms you are worried about? Is your cat eating, drinking, and toileting normally?
- Has your cats interactions with you changed are they withdrawn, aggressive or overly affectionate?
- Has anything changed in the household recently (for identifying any potential stressors):
-
- Visitors
- New pet in the house
- Change of routine
- Building work going on
- Moving to a new home
The differential diagnosis list will be driven by symptoms, a thorough history, and a clinical exam. Behaviors should be considered in terms of context, triggers, frequency, and duration. Remember, though, that common things are common if you hear hooves, think horses, not zebras!
Oral behaviors may be primarily related to gastrointestinal inflammation and diseases such as gastroenteritis, endoparasite burdens, pancreatitis, dietary intolerances, or inflammatory bowel diseases, which are more common than behavioral pathogenesis. Overgrooming, meanwhile, often results from pruritic skin disease and cannot be diagnosed without a complete skin workup. Alternatively, overgrooming can be due to pain, neurodermatitis or neuralgia, such as in the case of caudoventral abdominal overgrooming due to feline lower urinary tract disease or chronic pancreatitis.
Clinical exam and further testing
A thorough clinical exam is critical to diagnosis, as compulsive disorders are a diagnosis of exclusion.
The decision to carry out further testing, and which tests are appropriate, should be based on signalment, history, and clinical exam findings. These tests could include:
- Blood sampling
- A complete blood count (CBC), including biochemistry and hematology
- Hormonal testing (free and total T4)
- Allergy screening
- Skin examinations
- Tape strips, hair plucks and skin scrapes
- Microscopic examination of samples and the hair itself
- Cytology
- Allergy testing
- Imaging
- X-rays
- Advanced imaging, CT, MRI
TREATING COMPULSIVE DISORDERS IN CATS
After recognising the potential for compulsive behavior and eliminating any underlying or primary cause, a diagnosis of compulsive disorder can be reached. Treatment is based on an integrative approach, utilising behavioral modification techniques (standardizing husbandry, considering triggers and eliminating them where possible, and educating pet owners) and medical therapy. The aim is to reduce the frequency, intensity, and duration of compulsive symptoms to maintain a good quality of life.
Client expectations should be managed from the beginning to ensure you can develop trust to work together well as a team, especially as compulsive disorders are usually lifelong and managed rather than cured. These disorders are complex to treat due to their multifactorial etiology, so it is important that owners understand the diagnostic and treatment process so as not to become disheartened with outcomes or frustrated with progress. Success depends on client understanding, compliance and consistency.
WHAT DOES AN INTEGRATIVE APPROACH ENTAIL?
An integrative approach uses multiple modalities to address the symptoms of a condition to maximise the chances of a successful outcome. As compulsive disorders have a multifactorial etiology, it is often necessary to treat in combination with different departments of vets, and those offering complementary therapies (i.e. physiotherapists, acupuncturists, and behaviorists). As well, its important to consider concurrently prescribing different classes of medical treatment options to address all areas of the condition and improve patient outcomes.
A. BEHAVIORAL MODIFICATION AND ENVIRONMENTAL MANAGEMENT
- Set up a routine
- Reduce environmental stress
- Identify triggers and eliminate them where possible
- Ignore symptomatic behavior if feasible
- Consider enrichment
Working with a veterinary behaviorist is advised to support clients with making changes, observing their effects, and continuously modifying treatment plans in order to maximise success at treating compulsive disorders. Some techniques for behavioral modification and environmental management are detailed below:
- Set up a routine: This helps regulate the cats schedule, making it more predictable and eliminating anxiety triggers. Set a time for pet owners to feed their cats, even when the owners arent able to be around using automated feeders can help regulate this. Encourage owners to put aside some time each day to interact and play with their cats; this helps build their bonds and also adds structure and enrichment to the day.
- Reduce environmental stress: If owners are expecting a forced temporary change in their cats routine, such as building work or a temporary change in work patterns, they should try to keep as much as possible stable for the cat. If possible, have a partner remain constant, feed, and initiate play with the cat. In the case of building work, provide a safe, quieter area away from the work for the cat to be fed in.
- Identify triggers: Compulsive behaviors are often specific and contextual, meaning they may be triggered in specific places within the cats environment more than in others. It is important to identify situations, activities, or locations that trigger the behavior in order to be able to make efforts to block or remove them.
Make sure there are enough resources for the number of cats in the household. One of the primary causes of compulsive disorders is a cat feeling their needs arent being met. Make sure there are enough litter trays, access to food and water, toys, and scratch posts.
If there has been a change in routine, it can be reversed if its temporary, or medication/supplements can ease the transition to the new routine. Try to pre-empt these changes so they can be done slowly and with the right support.
- Ignore symptomatic behavior: Compulsive behaviors are often displayed during periods of acute conflict or high arousal. It is theorized that they develop as a coping or self-soothing mechanism. Attempts to use punishment or negative reinforcement exacerbates the problem by increasing the unpredictability of the cats environment, and may increase the conflict, high arousal, fear, and aggressive behavior triggering these disorders. Where possible, when theres no risk of safety concerns for the cat or owner, ignore the behavior to prevent accidentally rewarding it with attention.
- Consider enrichment: Inviting the cat to play, or distracting them by offering a change of activity, could be the release the cat needs to stop compulsive behavior and redirect it. Mental stimulation is a great way to prevent these behaviors from becoming chronic problems. Avoid laser pointers or blinking lights; these types of toys cause frustration because they simulate the cats natural hunting instincts of catching and killing prey, but prevent them from ever succeeding at catching and eating the prey.
B. MEDICATION
Few studies detail medication and its effects on compulsive disorders in cats. Therefore, there is no licenced medication used to treat these disorders. Any medication prescribed for the treatment of OCD in cats will be off-label and must be prescribed as per the veterinary cascade.
As in humans, medication use is aimed at treating the underlying neurochemical imbalance in the brain when an animal experiences an anxiety-associated behavior disorder. Medication is often lifelong; relapses are not uncommon when medication is ceased. Client expectations should be managed as such.
Although several antidepressant and anxiolytic medications are available, those showing the most efficacy for treating compulsive disorders in animals are clomipramine, amitriptyline, and fluoxetine.
Clomipramine is licenced to treat OCD in humans, and is a tricyclic antidepressant (TCA). Although the veterinary formulation Clomicalm (Virbac) is licenced for separation anxiety in dogs in the UK and US, it has also been approved for use in dogs with compulsive disorders in Australia and Canada. Studies have shown efficacy in cats also, but use in cats would be off-label and prescribed as per the veterinary cascade.
Clomipramine blocks the reuptake of serotonin and noradrenaline at synapses in the brain; there is also an anticholinergic effect due to antagonism of cholinergic muscarinic receptors. Increasing the levels of these neurotransmitters is seen to have the effect of regulating mood and behavior.
Clomipramine dosing is 0.25-1mg/kg q24hrs. A trial of two months is suggested, as it can take four to six weeks to take effect. If no clinical improvement is seen after two months, treatment should be ceased.
Side effects are rare and include vomiting, reduced appetite, and lethargy. Vomiting may be reduced by co-administration with a small quantity of food.
This drug should not be used in breeding males, pregnant females, lactating females or those with cardiovascular dysfunction or epilepsy. Care should be taken when prescribing for those with narrow-angle glaucoma, reduced gastrointestinal motility, or urinary retention.
Studies have shown the use of clomipramine to be superior to that of amitriptyline in dogs and cats, in treating OCD.
Amitriptyline is also a tricyclic antidepressant (TCA) but is not licenced for use in cats or dogs in any country, so it would be prescribed as off-label and as per the veterinary cascade.
Doses of 0.5-1mg/kg q24hrs are recommended. Side effects include frothing or foaming at the mouth on administration, drowsiness, GI disruption (constipation, diarrhea or vomiting) and odd behavior.
This drug should not be used in breeding males, pregnant females, lactating females or those with cardiovascular dysfunction or epilepsy. Care should be taken prescribing for those with narrow-angle glaucoma, reduced gastrointestinal motility, or urinary retention.
Fluoxetine (Reconcile, Prozac) is an anxiolytic in the class of selective serotonin reuptake inhibitors (SSRIs) approved for use in the treatment of OCD in humans. SSRIs increase the level of the synaptic neurotransmitter serotonin in the brain by inhibiting presynaptic serotonin reuptake, so more serotonin is available in the neural synapse to pass messages to nearby nerves. It is thought to have an effect on mood, emotion, and sleep. It can take four to six weeks for drug levels to stabilise, so cat owners should expect to dose for that long before seeing a significant change in the frequency and intensity of the compulsive behaviors.
Doses of 0.5-1mg/kg q24hrs are suggested. Side effects include loss of appetite, vomiting, decreased appetite, lethargy, restlessness, trembling and GI disturbances. Owners should be warned of a potential increase in aggression in response to medication. If side effects are severe or last longer than one week, the medication should be discontinued.
Fluoxetine should not be used in those with epilepsy or patients taking aspirin/anticoagulants, due to the risk of increased bleeding in the case of trauma.
Benzodiazepines (Diazepam, Xanax) are a group of medications that increase GABA activity within the central nervous system (CNS), resulting in anxiolysis and a range of cognitive effects, including the inhibition of memory. Best used for preventing acute fear-inducing event anxiety, they are particularly useful in cases where compulsive disorder triggers could be phobias.
Doses for Xanax are 0.125-0.25mg/kg as needed up to twice daily, while Diazepam is 0.5-0.2mg/kg as required. Side effects include sedation, muscle weakness and ataxia.
These medications should be avoided in patients with CNS or respiratory depression, severe muscle weakness, and hepatic impairment. They are not recommended in the treatment of long-term behavioral disorders due to the risks of disinhibition and interference with memory and learning.
Gabapentin is a structural analogue of gamma-aminobutyric acid (GABA) neurotransmitter. It was originally designed as an anticonvulsant but has been found to be more effective in the treatment of neuropathic pain and anxiety in humans and companion animals. In addition to its anticonvulsant properties, there are reports of a potential beneficial effect in the treatment of obsessive-compulsive disorders and self-mutilation in humans, and idiopathic ulcerative dermatitis in a cat. Doses of 0.5-10mg/kg PO q8-12hrs are recommended. Mild side effects are reported, including sedation and ataxia.
Other medications that can be used to treat the symptoms
caused by compulsive behaviors include:
- Glucocorticoids (steroid Prednisolone) For use as an anti-inflammatory in skin diseases; 0.5-1mg/ kg PO q 12-24hr taper to 0.5mg/kg q 48hrs.
- Antihistamines (Piriton, used off-label) 2-4mg/cat PO q8-12hrs. Used for the management of allergic disease.
- Non-steroidal anti-inflammatories (NSAIDS Meloxicam) Dose 0.05mg/kg PO q 24hrs (Robenacoxib) then 1-2mg/kg PO q24hrs for up to six days. Used to treat painful inflammatory conditions i.e. orthopedic (not advised in the case of GI pain or disturbances and not in conjunction with steroids).
- Ciclosporin (Atopica) For the treatment of atopic dermatitis at a dose of 7mg/kg q24hrs.
- Oclacitinib (Apoquel, used off-label) For the treatment of puritis associated with allergic dermatitis. Dosing 0.4-0.6mg/kg PO q12h for 14 days then q24hrs maintenance
It may be necessary to treat the symptoms of compulsive disorders, depending on the clinical signs, prior to dealing with the underlying disorder. For example, cases of OCD presenting with self-mutilation, injury to the skin, secondary infections and inflammation may need to be treated as these continue to drive the behavior and could now be a secondary trigger. Long term, I would expect the addition of symptomatic medication to be unnecessary as the incidence of the behaviors lessen.
Pheromones, including the feline facial pheromones, are detected by the cats vomeronasal organ, resulting in anxiolytic activity within the limbic system in response to threats to physical resources. They promote a sense of well-being in cats and come in the form of plug-in diffusers and topical sprays. They are good to use alongside behavioral modification and other prescribed medication.
C. FOOD SUPPLEMENTS AND NATURAL CALMING PRODUCTS
Prescription diets such as Royal Canins Calm contain hydrolysed milk protein and L-tryptophan to help soothe cats in stressful situations. Also containing psyllium to help control hairballs, and having a s/o index, they create an inhospitable environment for urinary stones to form, thereby helping with the common complications of a stressed cat. Natural dietary supplements (Zylkene, Calmex, Yumove calming care) are all advertised to support calming pathways in the brain and promote relaxation and happiness.
L-theanine An extract of green tea, thought to work by increasing serotonin, dopamine, and gamma-aminobutyric acid (GABA) levels in the brain.
L-tryptophan May reduce stress by altering bacterial populations in the gut.
Magnesium Prevents the buildup of cortisol and other stress-associated hormones, promoting calmness.
B vitamins Thiamine (vitamin B1) and vitamin B6 reduce stress by affecting neurotransmitters associated with anxiety and reducing cortisol secretion.
Melatonin Associated with the circadian rhythm, it is also involved in reducing stress.
Milk proteins Alpha-casozepine, a type of milk protein, is thought to bind to the same receptors used by anti-anxiety medications like diazepam, promoting calm.
Calming herbs
Chamomile Thought to work by altering neurotransmitter levels in the brain for example, by binding to the same receptors used by medications like diazepam.
Lemon balm Used in Yumoves calming care and other supplements, it reduces anxiety and improves overall mood.
Skullcap Used for centuries to reduce stress and anxiety, it may influence neurotransmitter levels within the brain, promoting stress relief.
Valerian root Very commonly used, and has been shown to promote happiness and calmness.
Other natural remedies to promote calmness
Flower essences Some calming products for cats include multiple flower essences. Rescue Remedy, which comes as a plug-in diffuser or spray, is a stress-relieving supplement containing the essence of five different plants:
- Helianthemum nummularium
- Clematis vitalba
- Impatiens glandulifera
- Prunus cerasifera
- Ornithogalum umbellatum
Catnip Available in many forms, including sprays, treats, and parts of the plant itself. It doesnt work for all cats, but for those it does, it creates a natural high, promoting happiness and relaxation.
Hemp oil Reportedly useful for pain management, anxiety and stress reduction, anti-inflammatory effects, epilepsy and seizure management, appetite stimulation and nausea relief in cats. Side effects include Gi upset, sedation, and changes in behavior such as pacing and restlessness. Little research has been done in this area, but hemp oil appears safe in cats at recommended dose rates.
D. COMPLEMENTARY THERAPIES
Physiotherapy
We are starting to explore and understand the many benefits and uses of physiotherapy in veterinary medicine. It is invaluable and has been used in cats with chronic pain or after significant musculoskeletal injury. Therapeutic massage could also have a role in treating some cats with compulsive disorders. It may be beneficial when the trigger is pain, allowing reduced use of medications; but also in receptive patients, where it could have a positive impact on well-being and stress reduction. Pet owners can be taught to practice therapeutic massage at home, which helps build their relationship with their cats, reduce stress and introduce therapeutic enrichment to the routine.
Acupuncture
Acupuncture treatments are shown to improve circulation, release hormones (endorphins), relieve muscle tension and stimulate nerves. It is usually well tolerated in feline patients. It is used for managing pain, decreasing inflammation, and reducing anxiety in cats. Studies have shown acupuncture to be an effective treatment for anxiety in humans, so we would also expect a good response in receptive cat patients.
WHY DO CATS DEVELOP THESE PROBLEMS?
Cats with compulsive disorders are thought to develop a trigger for the initiation of these behaviors. The trigger (or stressor) is often driven by environmental factors (a change in routine, limited resources, or a conflict of needs) or cat intrinsic factors (such as illness or injury leading to pain). Owner interactions have been found to exacerbate the condition in some circumstances. There could be a genetic component, as some breeds, such as Oriental and Asian breeds, are more commonly diagnosed.
Compulsive disorders are more common among indoor cats due to the stress of limited living space/territory and perceived confinement. Environmental changes are common stress triggers, including moving house or disruptions to the daily routine such as building work.
Compulsive disorders can be considered a coping mechanism developed when the cat perceives a frustrating situation, increasing anxiety levels, or a conflict with their needs.
The behavior can become chronic for many reasons:
- The trigger remains, leading to ongoing compulsive behavior
- The behavior itself can become self-soothing via the release of endorphins and dopamine; over time, therefore, symptoms can initiate without the need for the trigger
- The owner, likely unintentionally, reinforces the behavior by trying to prevent the symptoms with inappropriate interactions and distractions
CONCLUSION
Treating compulsive disorders can be a challenge and requires an integrated, multidisciplinary approach to achieve the best outcome. While it may appear that the incidence of compulsive behaviors decreases when pets are reprimanded a number of times, in reality they are simply removing themselves from view and committing the behavior elsewhere. Studies support the existence of this evasive behavior pattern, which could result in the underdiagnosis of compulsive disorders. The fact that cats are cognitive enough to understand and alter behavior patterns demonstrates the complexity of the condition, and explains why it can be so difficult to treat.
Treatment is likely to be a lifelong commitment for which success depends on client understanding, compliance and consistency in working alongside medical intervention and complementary therapists.